Robotics is a field that has advanced rapidly in the past decade, and which holds significant potential to transform key areas of healthcare and architecture. Aran Sena, a robotics expert within Foster + Partners, outlines which robotic systems can be integrated into future hospitals to address the complex challenges facing healthcare, and how this impacts architectural practice.
16th July 2024
Hospital Robotics: Designing for the Future of Healthcare
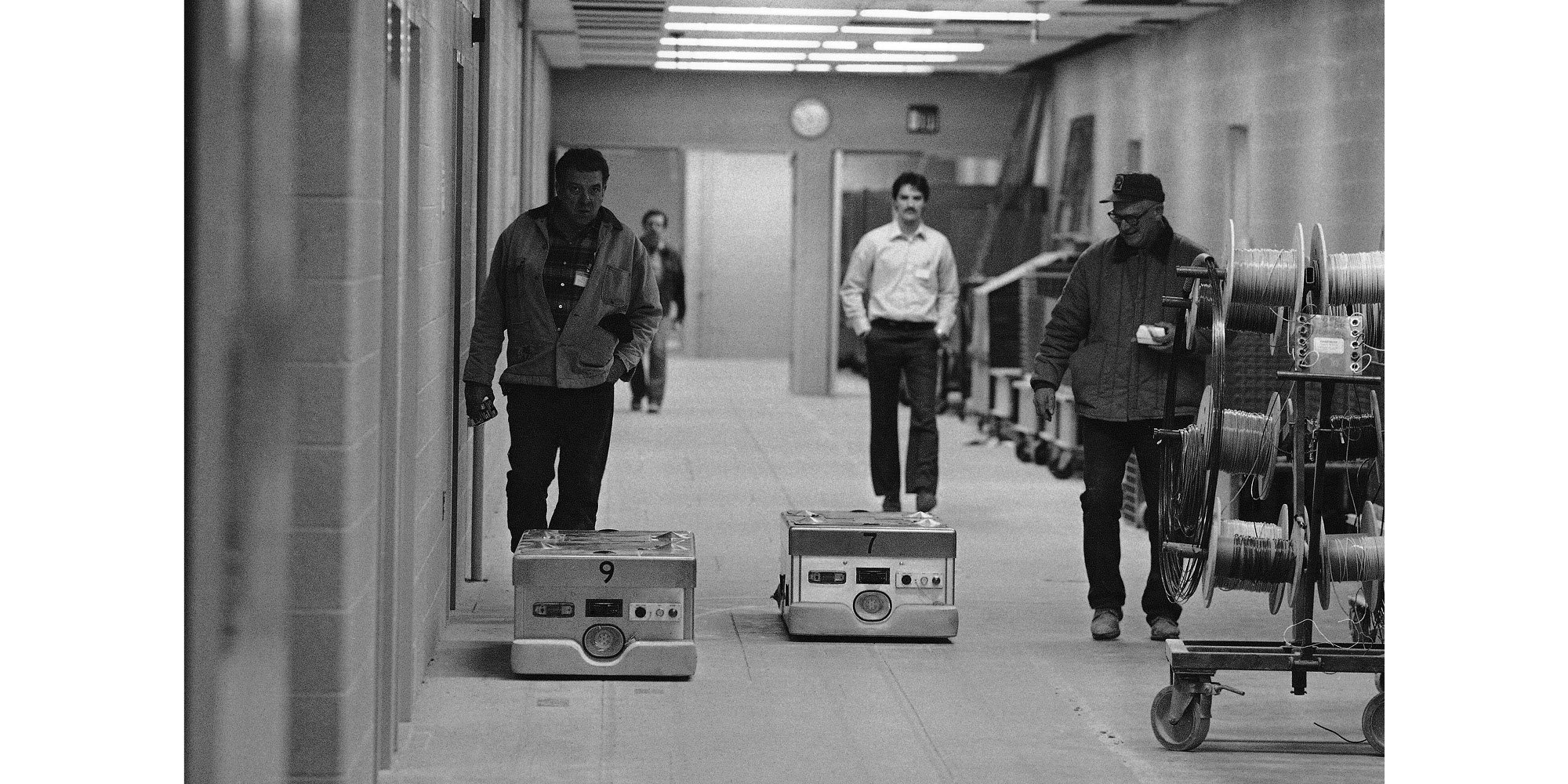
The use of robotics in hospitals – despite its futuristic associations – has been practiced for decades. The 1980s can be looked back on as the dawn of hospital robotics, where two key developments began simultaneously. The dawn of surgical robots saw researchers in California use newly available industrial robots to aid them in performing image-guided brain biopsies. Meanwhile, hospital planners – noticing productivity-focused innovation in the automotive industry – began exploring how robots might help improve the running of a hospital. During this time, one of the first hospital robotic delivery fleets was deployed at the University of Michigan’s Medical Centre, and was capable of running more than 700 errands each day, delivering drugs and equipment directly throughout the hospital via a dedicated robot elevator. The early developments seen over this period represent consistent themes in hospital robotics through to the present day: clinical care, logistics, and patient and staff support.
From the 1980s, developments in healthcare robotics were relatively slow and stable. A key breakthrough happened at the turn of the century, with the FDA approval of the da Vinci surgical robot system by Intuitive Surgical in 2000, which enabled complex minimally invasive surgeries. This system has benefitted surgeons as well as patients, enabling surgeons to work more precisely with less strain, and reducing pain, recovery times and stay durations for patients by minimising the site trauma required for a procedure. Additionally, the reduced human contact during surgery, small incision sizes required, and reduced quicker recoveries and discharge all help to reduce risks of both surgical site infections (SSI) and healthcare associated infections (HCAI).
The rise in computational power and artificial intelligence over the past decade, alongside widespread public and private investment in robotic infrastructure across scales, means we are at an exciting inflection point. The field of robotics has greatly diversified, with robotic systems becoming more cost-effective, and increasingly applicable across a variety of healthcare roles and services. The question for healthcare designers, then, is how to integrate this rapidly expanding field into hospitals in ways that can respond to both the daily and long-term pressures of healthcare provision.
Types of healthcare robotics
Hospital robotics encompasses a breadth of services and systems. These can be categorised in three domains: clinical care, facilities management, and supply chain automation.
The first, clinical care, includes a wide range of robotic services in the hospital that can be considered in terms of direct clinical care and clinical care support systems. Direct clinical care includes robotic radiotherapy systems that enable more comfortable treatment positions, and rehabilitation and mobility systems that help patient's achieve improved outcomes and independence.
Clinical care also encompasses surgical robotics, which enhance surgeon's precision with less strain and reduce patient recovery times and infection risks. What began as general surgery - originally dominated by the da Vinci system - has since evolved into an ecosystem of robotics developed by numerous companies for a wide range of procedures (such as orthopaedics, neurosurgery, and ophmology). Over the past decade, robot-assisted surgeries have increased from 1.8% to 17% globally, with robotic surgery becoming the standard in particular domains – with 85% of prostate surgeries being performed with robotic assistance in the USA.
Automated test tube handling using Universal Robots UR5 arms and advanced vision © RoboMinds
A second category of robotics is facilities management, which covers the maintenance of the hospital environment. The NHS states that facilities managers ‘ensure that the services that patients need during their stay in hospital are available, such as meals, linen, and a clean environment’; many of these processes can reasonably be automated or assisted with robotics. Cleaning robots, for example, can work alongside staff, deploying UV light, vacuum, or aerosol technology to disinfect and sterilise spaces, and transport and security infrastructure can enable easier access to healthcare facilities, which reduces patient and family stress when arriving and departing from the building.
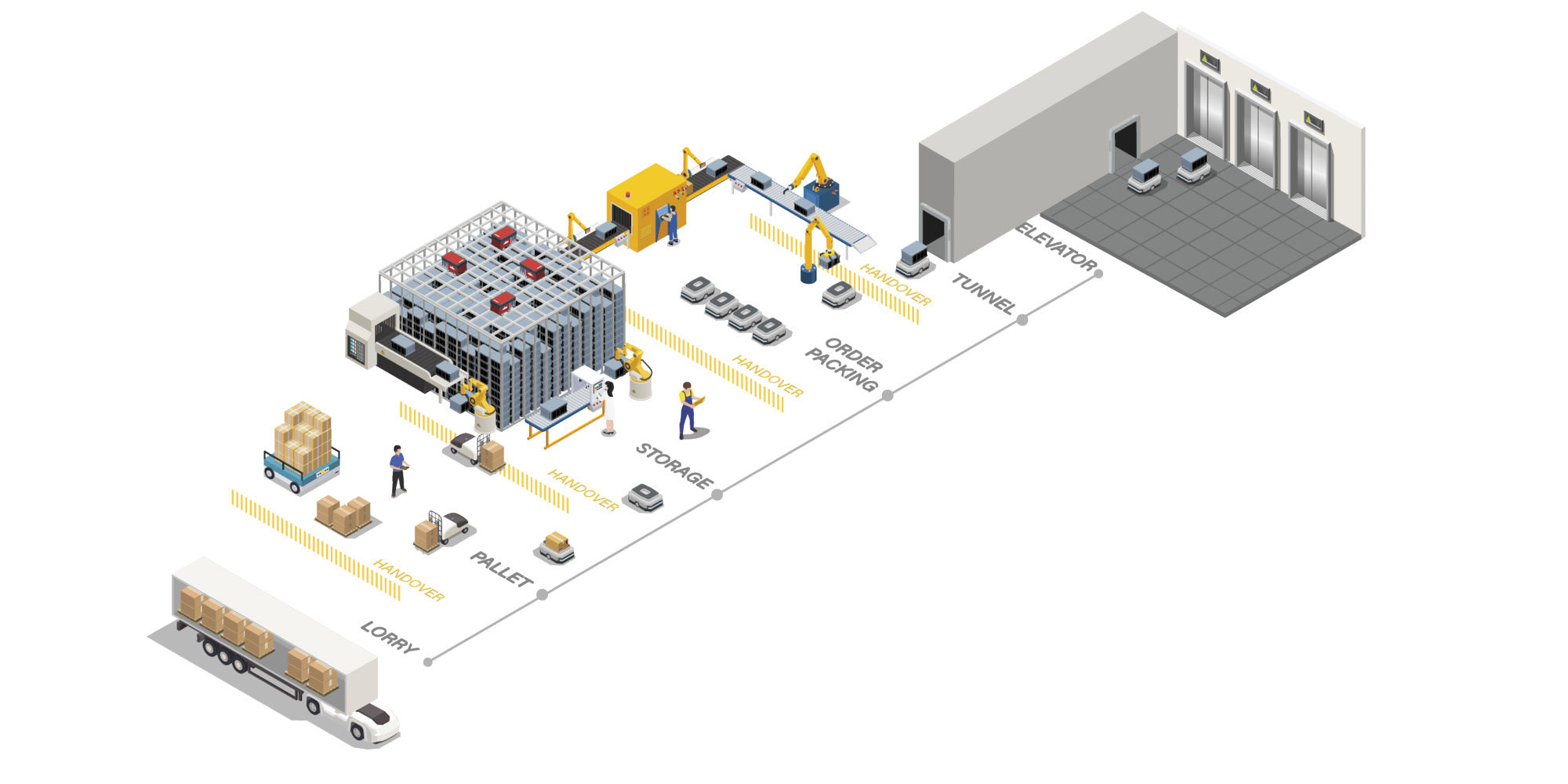
The third significant category of robots in hospitals covers those involved in the automation of hospital supply chains. Hospitals depend on the movement of vast quantities of supplies, food, and waste to function, conventionally depending on large porter services teams for the movement of larger goods, and fixed infrastructure such as pneumatic tube systems to move smaller items such as laboratory samples. Increasingly, robotic goods handling fleets are being deployed in hospitals to alleviate the stress on staff, improve efficiencies, and improve the flexibility and adaptability of supply chains.
Robots have long demonstrated their value in supply chains, with automated guided vehicles (AGVs) having been in use for decades – as they were in Michigan in the early 1980s. AGVs follow established routes and markers, typically in ‘off-stage’ areas away from the public and patients. Advances in sensing, obstacle detection and navigation resulted in a new category of delivery robot, the autonomous mobile robot (AMR), which sense the world around them and respond accordingly, allowing them to deliver supplies directly to and from nursing stations or even patient rooms. Recent advances in humanoid robotics has proved particularly exciting, with many companies seeking to fill gaps in logistics automation across industries.
Supply chain automation also extends beyond the wards and corridors of the hospital to surrounding networks. Integration with off-site services has led to the use of service tunnels to link campus buildings, saving space in main hospital structures, and soon aerial services such as delivery drones will help to rapidly and efficiently link hospitals to wider communities and services.
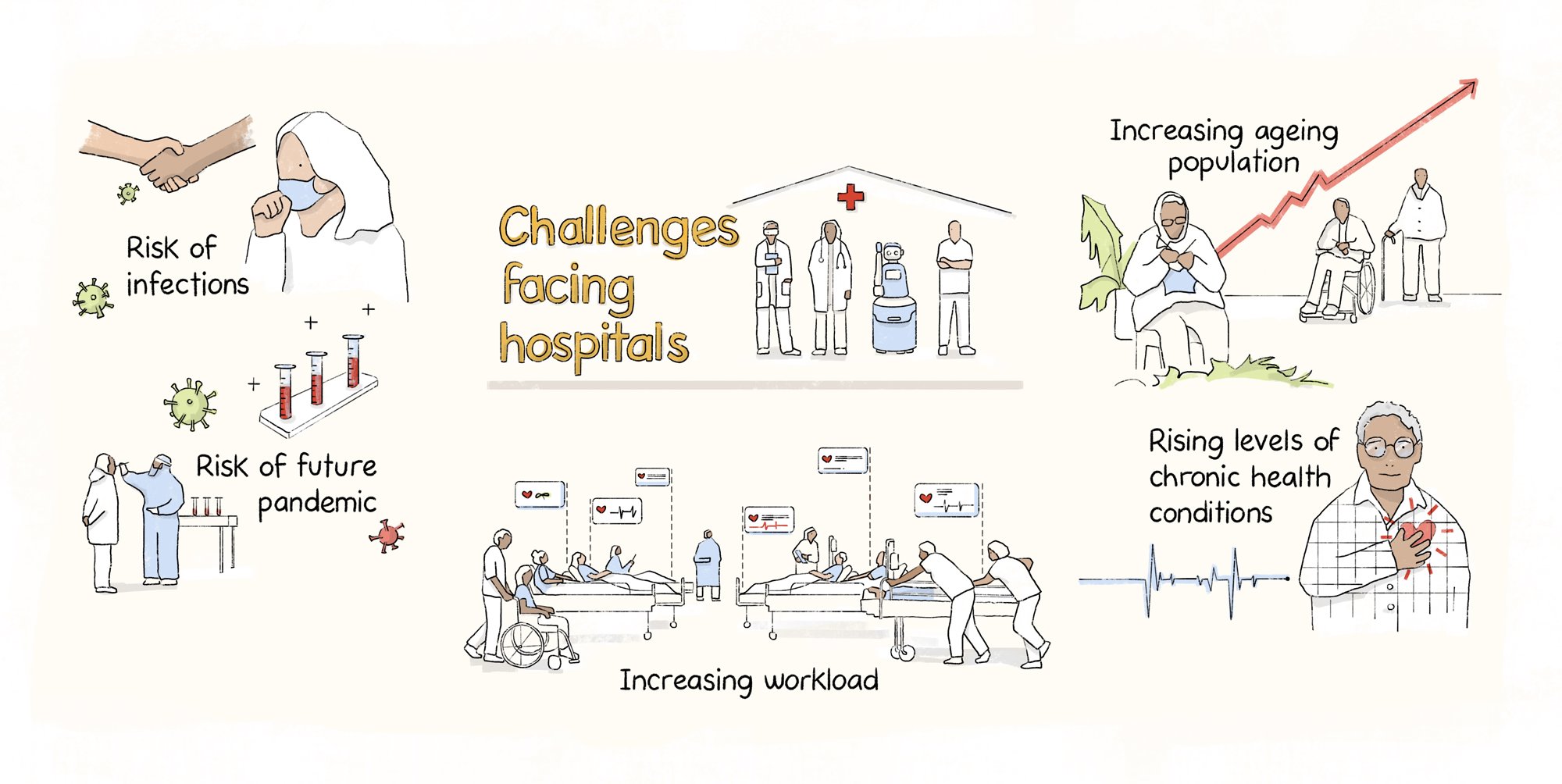
Challenges facing healthcare
As robotics has developed, the challenges facing healthcare have also grown more complex – with the recent coronavirus pandemic starkly exposing the precarity of healthcare systems and the continued need for intelligent hospital planning. There are multiple crises facing hospitals today: increases in demand exerted by an ageing population and rising levels of chronic health conditions; pressures on staff due to labour shortages, insufficient resourcing, and increased workloads, leading to physical and mental health issues such as burnout and moral injury; and the increased risk of healthcare-associated infections (HCAIs) as well as the rising risk of future pandemics. These problems are interlinked, with the rise of one issue exacerbating others. This requires systematic change to resolve and cannot be addressed by design alone. However, designers do have an ability to steer outcomes, and a responsibility to offer practical and creative solutions wherever possible.
Hospitals face a wide range of complex and interlinked challenges. Robotics will play a pivotal role, not only in elevating patient outcomes by delivering the highest quality of care, but also in enriching the experiences of patients, caregivers, and staff.
Meghna Purkayastha, Healthcare Designer, Workplace Consultancy
Altogether, this array of systems can respond to demand (supply chain automation and nursing assistance robots), control cross-infection (cleaning and testing), care for complex illnesses (surgical and imaging technology), and support patient wellbeing and recovery (nursing assistance, medicine delivery, and physiotherapy robotics), as well as improve overall patient experience by catering to a person’s needs throughout their stay (scheduling, food delivery, entertainment services, supporting social interaction).
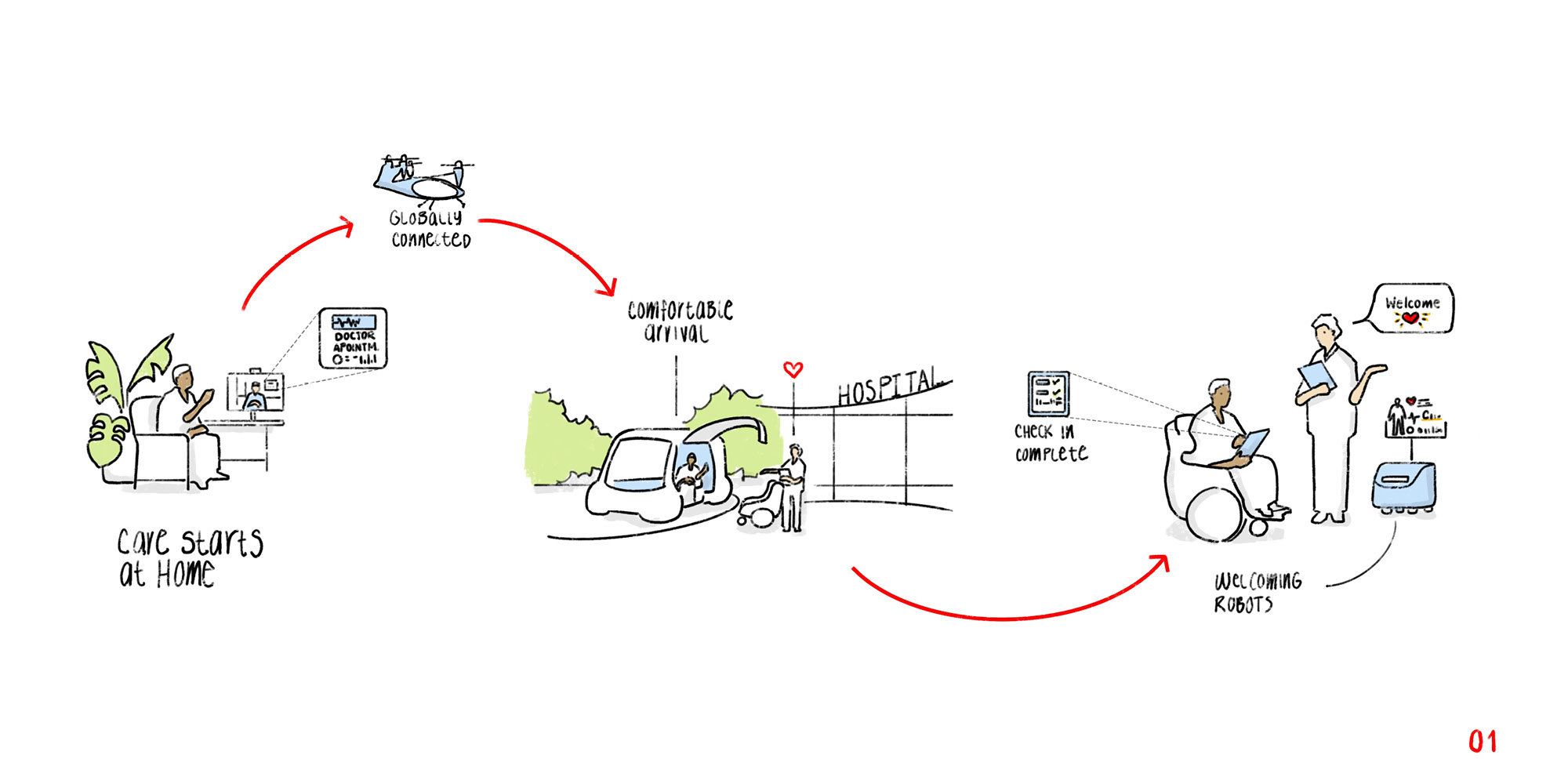
In a future scenario, these robotic systems could touch upon and transform every stage of the patient journey and staff experience. Healthcare robotics can empower healthcare professionals to give more direct care to patients by freeing them from routine tasks and contribute positively to clinical outcomes and personal wellbeing. Some of these strategies will be familiar, others more revolutionary.
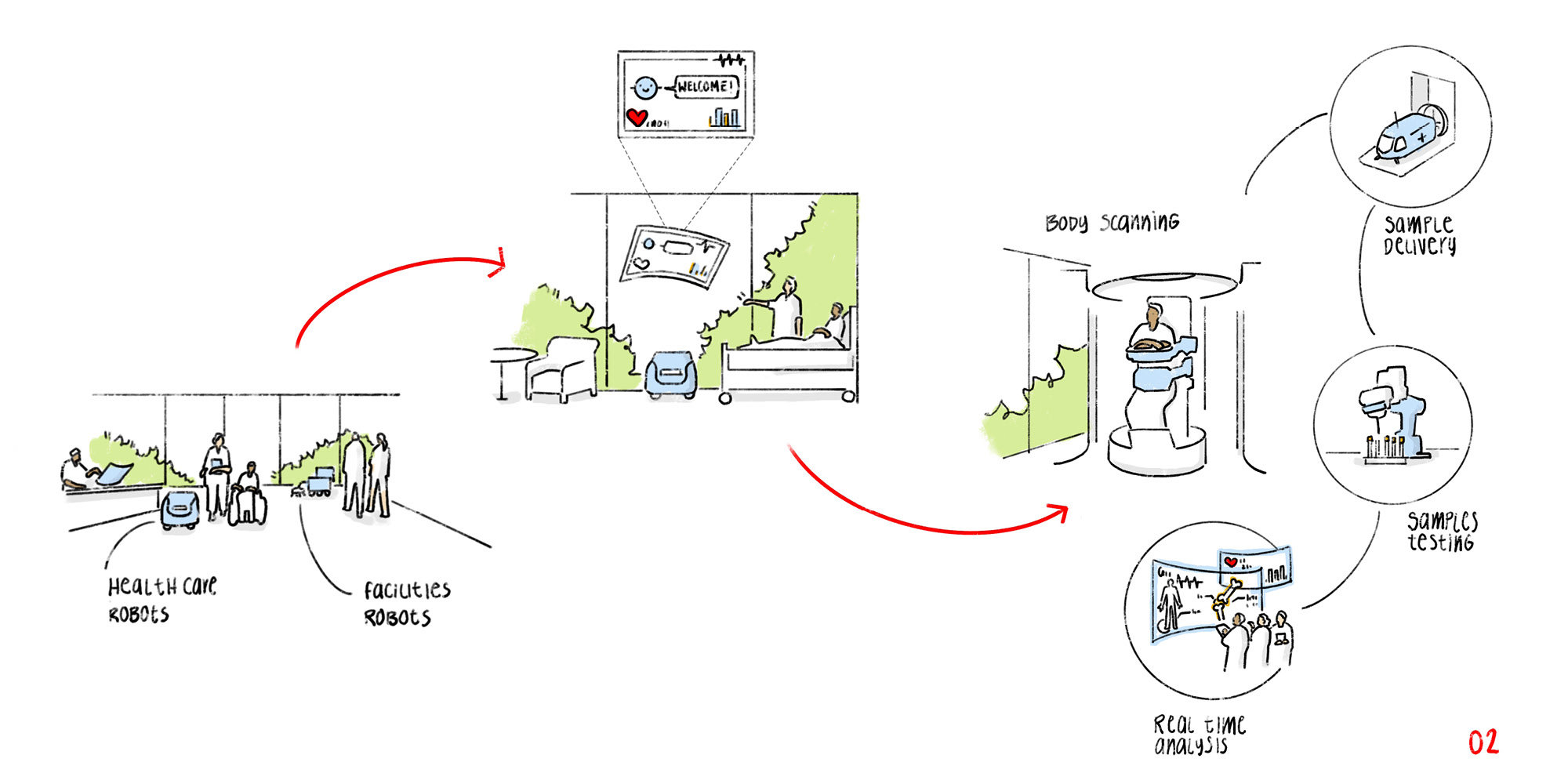
The following slides outline a patient journey where robotic systems are integrated.
SLIDE ONE: The patient discusses a treatment plan with their doctor to reduce pain related to a chronic condition with their spine. They talk conversationally, with the Doctor’s AI assistant taking the required notes as they talk, and making the required bookings for transport, diagnostics, and surgery. Transport to the hospital is complicated by the patient being unable to drive due to their condition, and living in a remote location with no available public transport routes. An eVTOL transport is arranged to bring the patient to a nearby vertiport, with final transport to the hospital by driverless car. The patient is welcomed by a porter, who accompanies them to their room with the assistance of an autonomous wheel chair for the patient and a mobile robot for their luggage. © Foster + Partners
SLIDE TWO: The porter briefs the patient on the agenda for their stay. The corridors are calm, quiet and spotless, with just a few cleaning robots making their rounds, and patients walking with their visitors. Before surgery, healthcare staff require accurate imaging for procedure planning, and blood tests to ensure that the patient is fit for surgery. The patient receives CT scans in a comfortable room, while previously collected blood samples are flown to a nearby district central laboratory for analysis. Soon after the scans are complete, the surgical team agree a procedure plan with in collaboration with their AI powered planning system, and receive the all-clear to proceed from the laboratory. © Foster + Partners
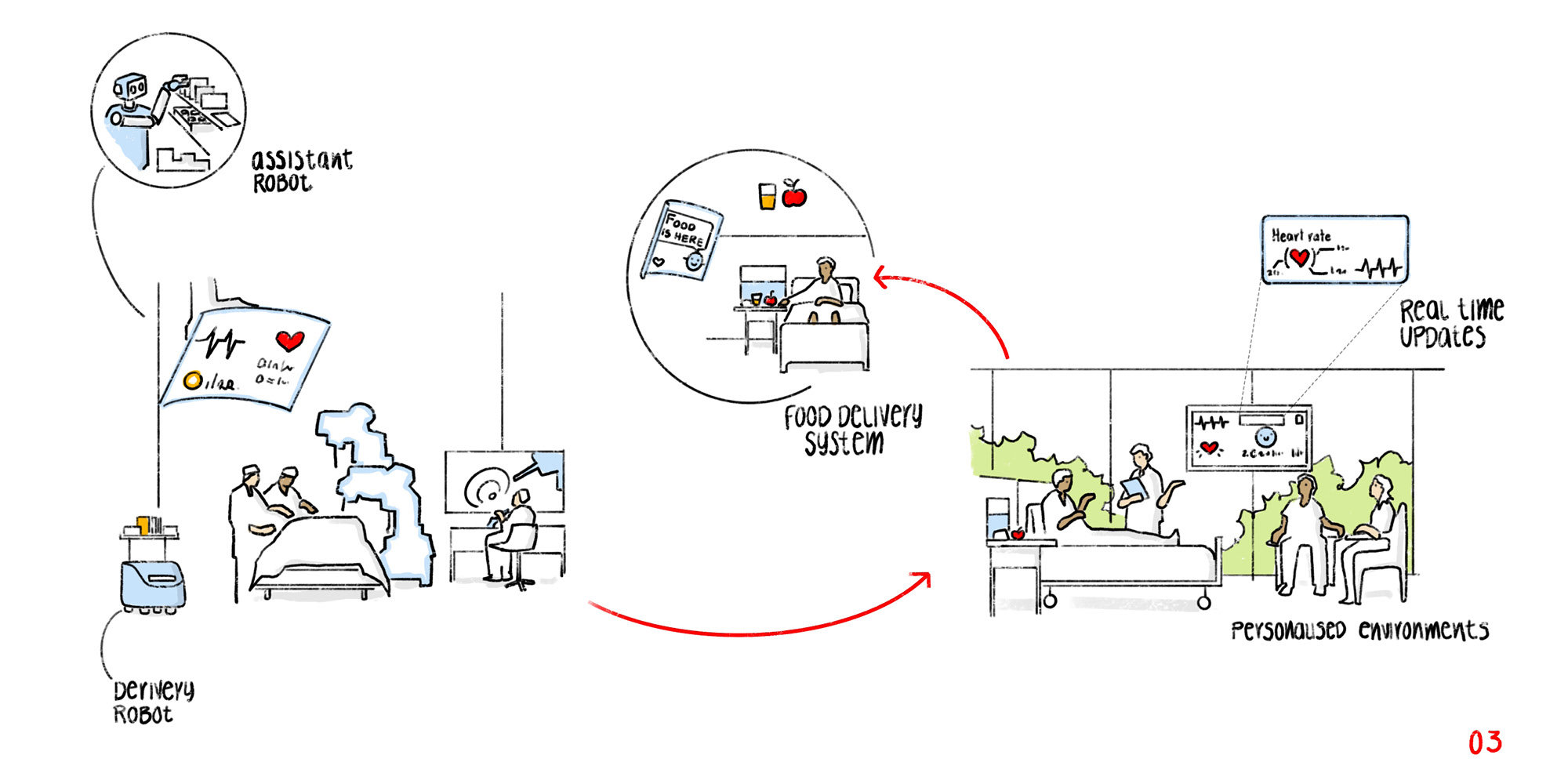
SLIDE THREE: Surgical equipment is prepared and brought from an off-site logistics centre to theatre by an end-to-end robotic supply chain. The first time the equipment is exposed to people is when it is unpacked by the surgical team. A mixed team of expert surgeons, nurses and robots perform surgery, with a procedure plan that minimises risk and recovery times. Following a successful surgery, the patient begins the recovery process, with the benefits quickly noticed through significantly reduced pain. A curated, personalised meal plan is autonomously prepared and delivered to their room when they feel ready to eat, and their recovery is closely monitored through a variety of in-room and wearable sensing, to help detect any complications such as infection from surgery early-on. © Foster + Partners
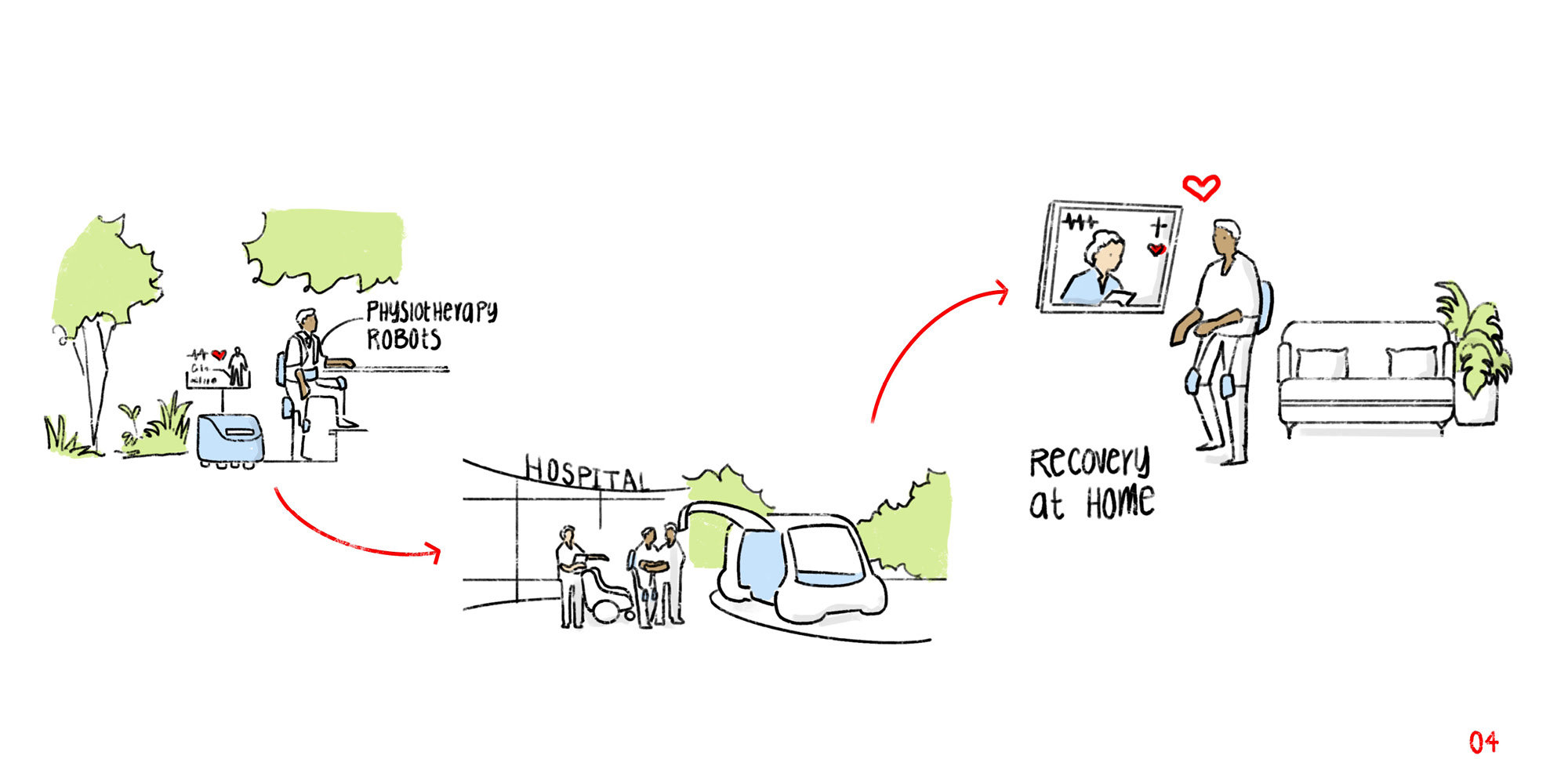
SLIDE FOUR: Once the patient has recovered from the immediate effects of their surgery, they begin their rehabilitation plan with the help of a robotic exoskeleton. This robot-assisted therapy, combined with remote monitoring of the exoskeleton’s motion and frequent check-ins from the patient's local healthcare team have helped to significantly improve their mobility and reduce symptoms. This has resulted in a significantly improved quality of life and a return to relative normality for the patient. © Foster + Partners
Towards a design methodology
For architects, the question is how to make this patient journey possible. It is no longer enough to design for a single, specific robot; a more holistic, network-like approach is needed. Hospital design must take place across scales – from the smaller interior details of a patient room, through the form and layout of the building, to questions of connectivity at a citywide level. Given the extensive planning and construction period that is typical for hospitals (during which time technologies can rapidly advance), the long service lifespans of hospital facilities, and the ever-shifting demands and challenges placed on them, this is a remarkably complex task.
Designing with intent is key if robots are to be properly integrated into the hospital and its web of processes. To do this, architects must call upon a wide range of expertise – from robotics to healthcare specialists to accessibility experts – to consult on the planning and infrastructure of the hospital. Design limitations becomes increasingly costly to correct the later in the process they are addressed. At worst, a failure to design with robotics in mind might entirely omit the opportunity to introduce them in the future.
Robotics and floor plans
Mobile robots can notably alter spatial layout: corridors need to be wide enough to allow for a robot and an emergency hospital bed to pass simultaneously, and rooms need to provide enough space for turning. Evacuation pathways must also be planned carefully, and mobile robots should be programmed to avoid escape routes so that the risk of them obstructing people in an emergency is reduced. Even door layout can affect the efficiency of robots, impacting both delivery time and construction costs. Similarly, handover areas need to be carefully choreographed so that the sending and delivering of goods remains safe, accurate, and reliable. Spaces for storage, charging, and servicing also need to be allocated, and in such a way that robots do not unnecessarily interfere with people's wellbeing.
Advances in clinical care robotics mean that some clinical care systems, rather than being confined to a specialist room, are increasingly mobile and can be moved between rooms - potentially freeing up space in the floor plan. Designers need to account for this rising flexibility, and plan patient rooms that can adapt to different clinical care scenarios.
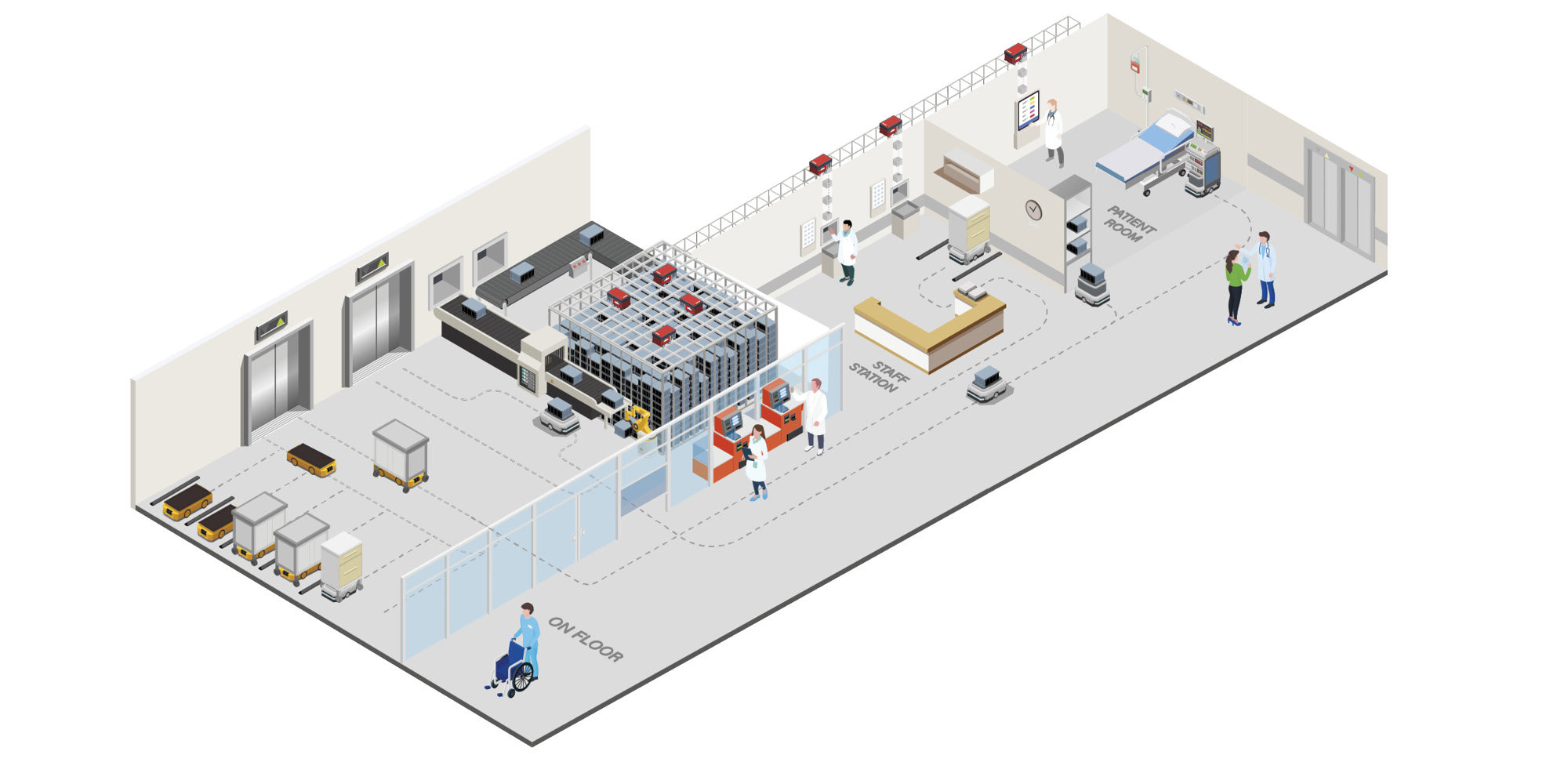
When robots move from ‘off-stage’ to ‘on-stage’ it is vital to consider when and how they will interact with patients and staff, and how this will be modelled and controlled. Here, delivery routes to staff stations and patient rooms are displayed with a variety of goods transport options from conventional AGVs to integrated robotic goods handling systems. © Foster + Partners
A key consideration when integrating robotics is whether a robot will be patient-facing or not. Robots that operate exclusively in ‘off-stage’ areas can benefit from more controlled environments and will typically operate with and around staff who can be trained on how to work with them safely. Robots that will operate in patient-facing, ‘on-stage’ areas face the challenges of unexpected obstacles and unplanned interactions, and in turn become obstacles to other people as they move around.
Robotics and building form
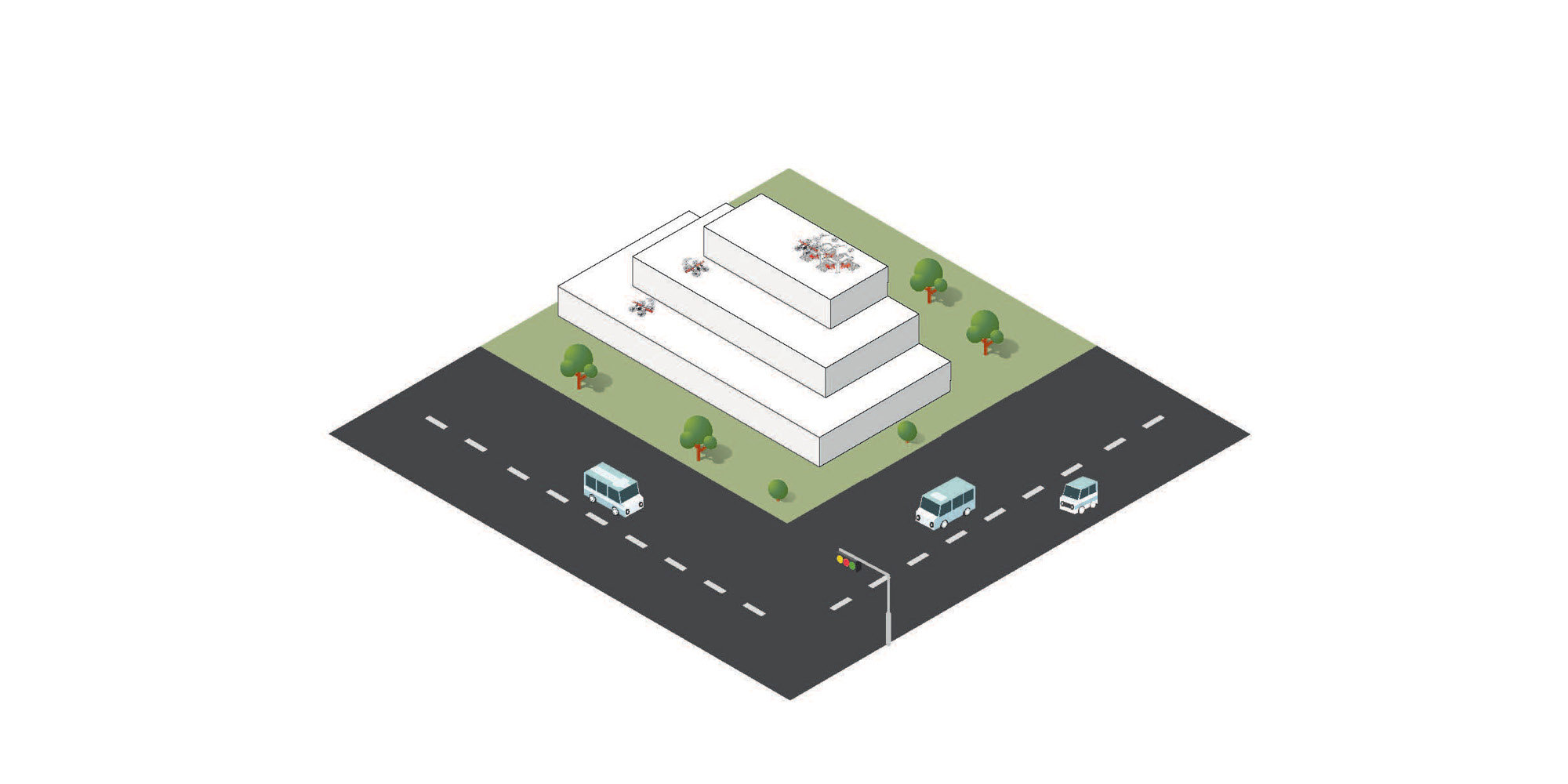
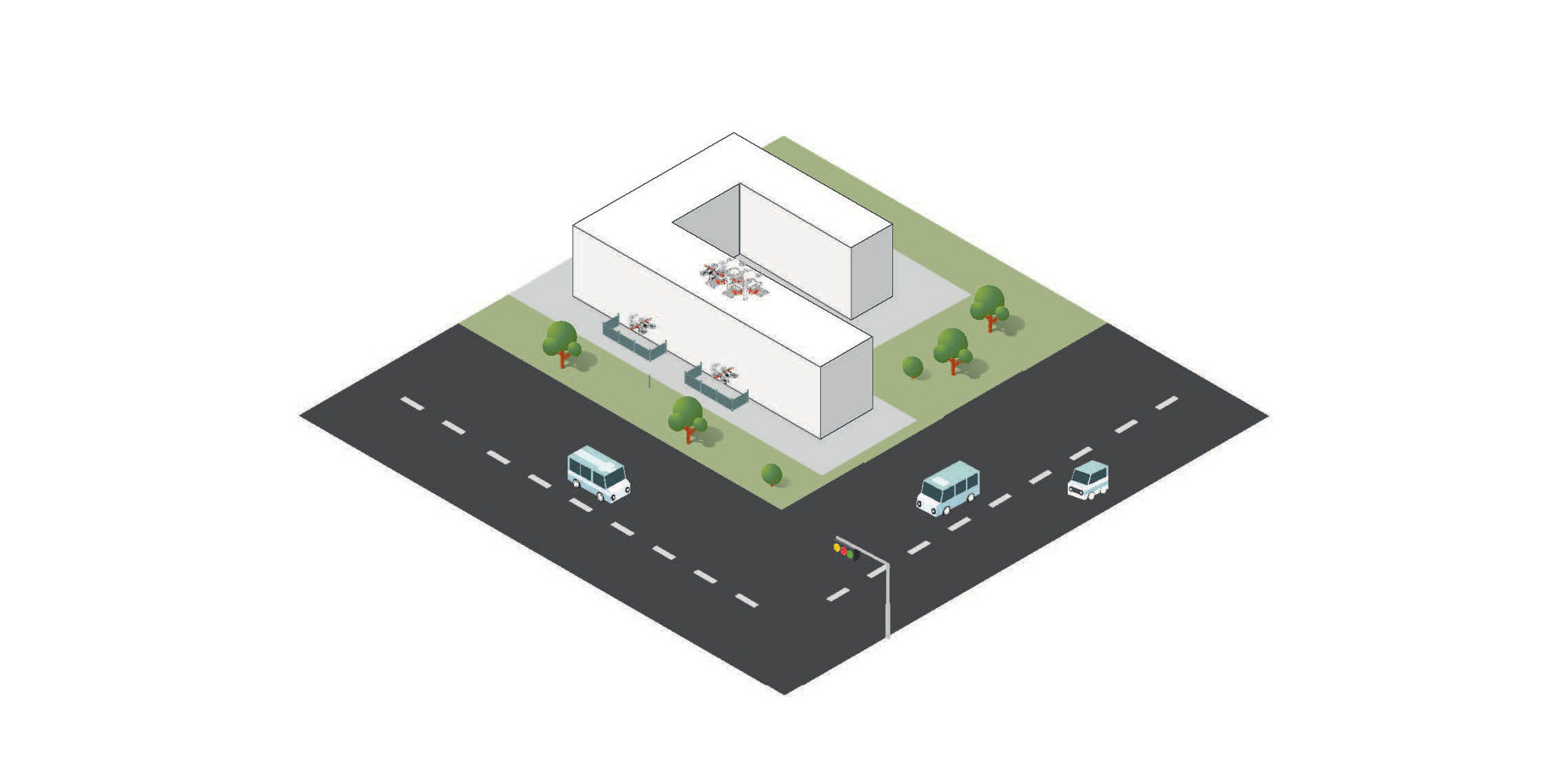
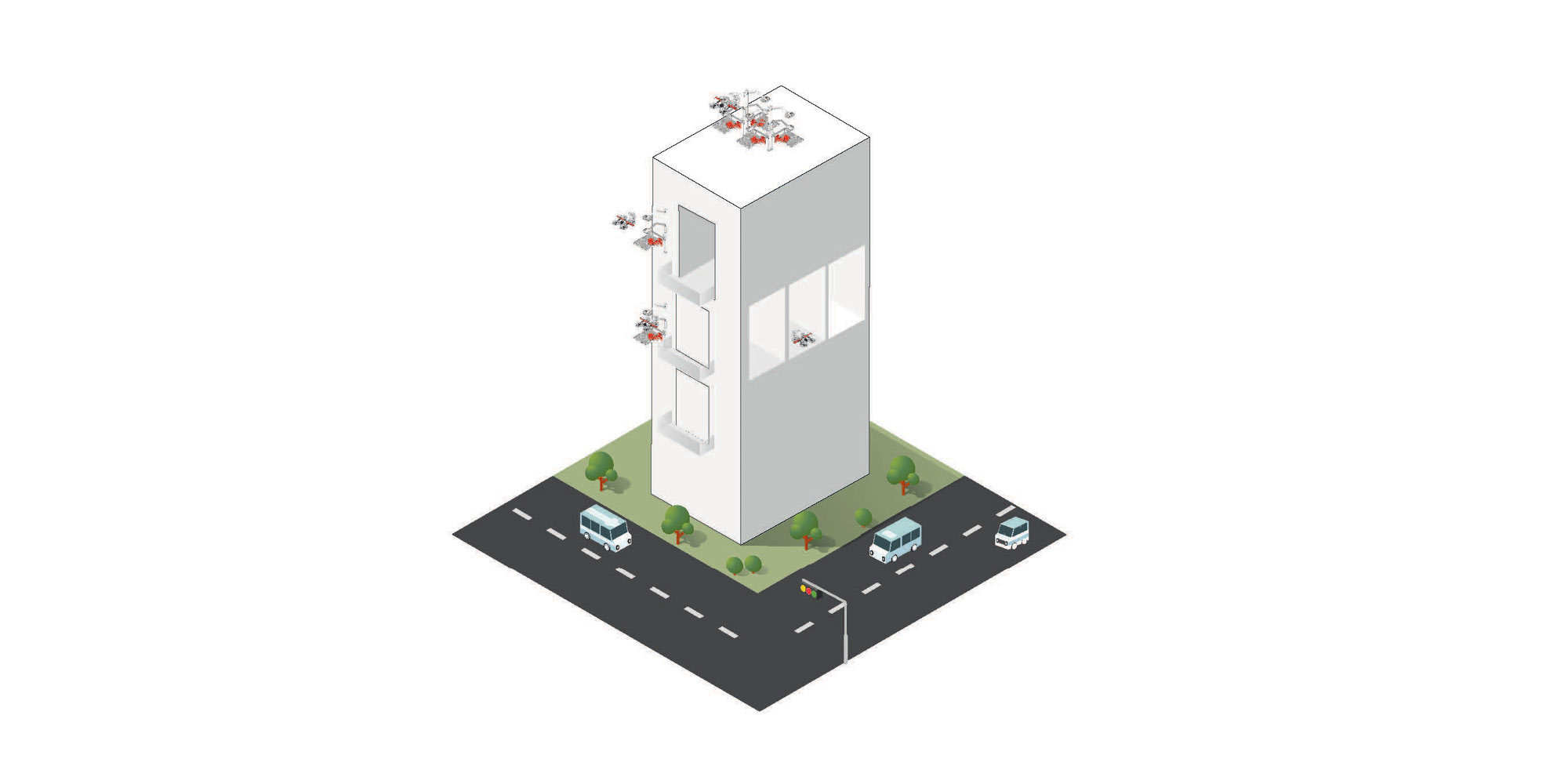
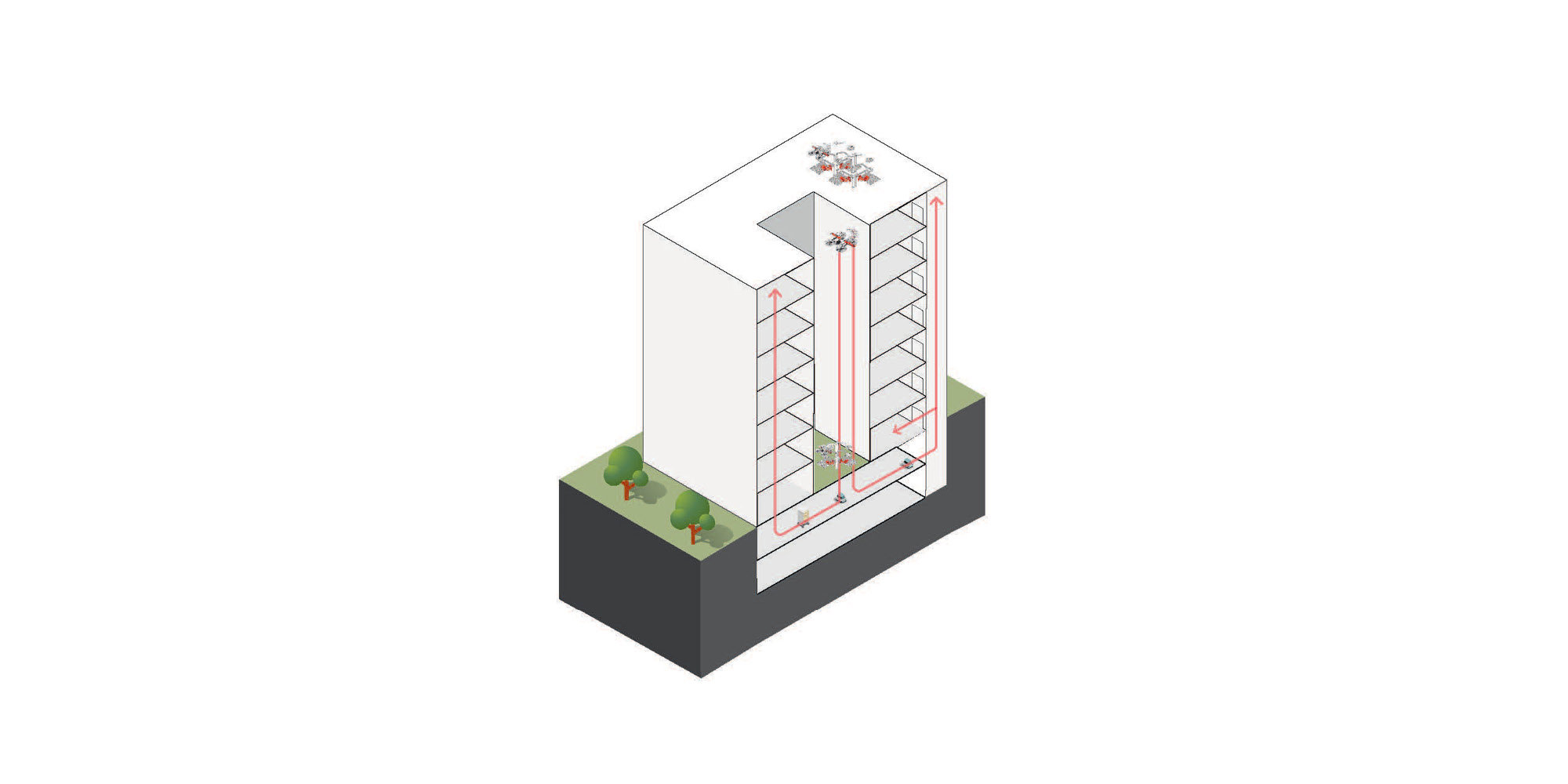
The form of a hospital building also has major implications for the integration of robotic services. The choice between high-rise and low-rise structures will impact the planning of drone delivery integration, and internal goods handling systems' path planning and delivery times. Often, forms are steered by contextual factors such as the surrounding urban fabric and planning codes that endorse one over another; however, within the broad categories of high-rise and low-rise, certain design choices can impact the opportunities for robot integration.
The integration of mobile robots is influenced by form. Internally, low-rise buildings will tend to result in longer travel distances for both people and robots, as hospital services spread out, but can benefit from below-grade movement via tunnels to connect different areas in the hospital and facilitate safe and rapid robot movement. High-rise, in contrast, tends to have shorted travel distance, but is constrained by a need for elevators to provide vertical movement.
Drone delivery is also dependent on building form. Roof-level and ground-level package handover between drones and staff is not ideal as it can result in longer walking distances and retrieval times - with ground-level delivery raising particular security and safety concerns. For designers, there are many potential approaches for deeper integration of drone deliveries. A low-rise building profile with a stepped roof increases the landing space available for drones, and allows staff on each floor to access drones to exchange goods. However, a stepped roof cuts into the floor plan, and an increase in landing space for the drones results in a decrease in floor space – which likely impacts the number and layout of patient rooms. Another low-rise building profile, without a stepped roof, has a different set of outcomes: while the floorplan is more effective, the roof space and therefore landing space for drone delivery and handover is limited.
In high-rise contexts, facade-level integration can be achieved through features such as balconies or garage openings, but these can still be on the periphery of where staff and patients are located. Delivery deeper into floorplans would enable more convenient parcel handovers, but poses a greater challenge. Drop-shafts from roof-level delivery points address upper-levels of the building, while other options for lower level floors include allocating intermediate service levels, perforating the building structure to create drone access space, or creating a handover point to the internal goods handling robots at a convenient location such as the basement. This improves the speed of parcel handover, by bringing deliveries closer to their destination. Designers must carefully consider these options, as they involve a trade-off between clinical and non-clinical services.
These differences in building form do not only impact robotic services: they impact accessibility and wayfinding, light and ventilation, patient and staff experience, and construction and operational cost. Healthcare planning is always a practice of compromise and solution, where a hospital's many requirements should be considered at once.
Masterplans for healthcare
Healthcare is increasingly distributed, with diagnosis and treatment beginning in patients’ homes, and advancing capability in community centres and specialist care centres. Operational support for hospitals is also becoming increasingly distributed, helping healthcare networks to operate more efficiently by sharing resources and services. This requires interconnection at a digital and physical level where designers can consider drone routing (that are conscious of range limitations, airspace restrictions, and weather conditions) and other future forms of autonomous transport, to deliver a future healthcare system that can address rising challenges in healthcare, accessible to both urban and rural communities.
Human-robot interactions
Hospital design should not only consider the different scales at which robotics can be integrated; it must also absorb questions about human behaviour and how the same space will be used by a range of occupants. Firstly, architects need to consider how interactions between humans and robots should be structured. As Julie Shah and Laura Major propose in What to Expect When You’re Expecting Robots, we need to think of robots not as adversaries but as social entities that we should learn to work alongside; we are designing ‘not for but with’ robotics. Designing ‘with’ is a powerful concept; robots should be geared towards solving some of the core problems facing healthcare provision and improving the experience of a hospital for those who use it. To do this requires a social shift towards the acceptance of these systems – one built on trust and a widespread knowledge of how these systems work.
Secondly, the broadening of what – and who – we are designing for engages with questions of accessibility. By thinking about how robots and people might work best together, a more nuanced and resilient design strategy emerges. Interestingly, an accessibility-led approach is often compatible with designing for robotics: both challenge our assumptions about how space is interpreted and navigated. Hands-free and step-free access, well-lit corridors, and clear wayfinding are all design decisions that improve mobility for humans and robots alike (as well as reduce the spread of pathogens via surface contact). Ultimately, these design choices are often mutually beneficial to robots and people.
Designing truly inclusive spaces for a diverse range of human needs makes for more resilient, futureproof buildings. While innovative technology and robotics is extremely exciting for hospital design, we must remain mindful of considering patient and disability-led perspectives along the way, to ensure that the full range of experience is accounted for.
Suzan Ucmaklioglu, Inclusive Design Specialist, Technical Design Group
Finally, we must not forget that hospitals are places for care and healing (as well as research and innovation) and are where patients and their families might be at their most vulnerable and distressed. As always, people-centred perspectives must be brought to hospital design and find ways to intersect with innovative technology in ways that improve wellbeing. It would be inappropriate and unrealistic, for example, to automate all patient interactions with staff. Robots and humans tend to be good at different things – an observation which should be remembered even as integration and collaboration is encouraged.
Hospital of the future
Equipped with an ecology of approaches, and applying much of the thinking discussed here, Foster + Partners is currently designing Mayo Clinic in Rochester, Minnesota. Designed with a methodology rooted in interdisciplinarity, the Mayo Clinic will adopt a universal grid, along with generous floor-to-floor heights, that will allow clinical spaces to change over time and respond as healthcare continues to evolve. Care environments will be served behind the scenes by highly flexible technological infrastructure containing mechanical, data and robotic delivery systems that support pioneering treatments while allowing prioritisation of human connections. The seamless integration of digital capabilities blurs traditional distinctions between inpatient, outpatient, and virtual care to support patients throughout their healthcare journey.
Visualisation of Mayo Clinic Campus & Hospital of the Future, Minnesota, United States. © dbox / Foster + Partners
Visualisation of Mayo Clinic Campus & Hospital of the Future, Minnesota, United States. © dbox / Foster + Partners
Architecture, robotics, healthcare
The potential to transform healthcare through design is both incredibly exciting and demanding in its complexity. The collaboration of architects, healthcare specialists, and robotics experts early on and throughout the design process is essential if design teams are to deliver the future of healthcare.
Author
Aran Sena
Author Bio
Aran Sena is a Design Systems Analyst working in the Specialist Modelling Group at Foster + Partners, where he advises on how robotics and autonomous systems can be applied in architectural practice. Aran obtained a PhD from King's College London where he researched methods for robot control and human-robot interaction. After completing his post-doctoral position at Imperial College London, Aran joined the practice in 2023.
Editors
Tom Wright and Clare St George